Preventive Healthcare
Paraplegia: Causes, Rehabilitation & Life After Spinal Injury

Table of Contents
- What is Paraplegia?
- How is it different from other forms of paralysis?
- How does the location of a problem affect paraplegia?
- Causes of Paraplegia
- Non-Traumatic Causes
- What are common risk factors for developing paraplegia?
- Signs and Symptoms of Paraplegia
- Diagnosis and Tests
- Rehabilitation and Treatment Options
- Living with Paraplegia: Daily Life & Emotional Well-being
- Support Systems and Resources
- Prognosis and Long-term Outlook
- Conclusion
- FAQs
What is Paraplegia?
Paraplegia is a type of paralysis that affects the lower half of the body, typically resulting from damage to the spinal cord in the thoracic, lumbar, or sacral regions. It impairs motor and sensory functions in the lower extremities, making it difficult or impossible for individuals to walk or stand. Imagine not being able to feel or move your legs – this is the reality for many people living with paraplegia.
Paraplegia can be classified as:
- Complete paraplegia: Total loss of motor and sensory function below the level of injury
- Incomplete paraplegia: Some motor or sensory function remains below the affected level
The severity and extent of paralysis depend on the location and completeness of the spinal cord lesion. With incomplete paraplegia, one may retain some movement or sensation in the legs, while complete paraplegia results in total loss of voluntary motor control and feeling.
How is it different from other forms of paralysis?
Paraplegia specifically impacts the lower extremities, distinguishing it from other types of paralysis:
- Quadriplegia (tetraplegia): Paralysis affecting all four limbs – both arms and both legs
- Hemiplegia: Paralysis on one side of the body, impacting one arm and one leg
- Monoplegia: Paralysis limited to one limb, usually an arm or leg
While these forms of paralysis have some similarities, the term "paraplegia" is used when the impairment is localised to the lower half of the body. Paraparesis refers to partial paralysis or weakness of both legs, but not a total loss of function.
How does the location of a problem affect paraplegia?
The manifestation of paraplegia significantly depends on the level and extent of the spinal cord damage. The spinal cord is divided into segments, each controlling specific functions:
- Cervical (C1-C8): Neck and arm movement, breathing
- Thoracic (T1-T12): Trunk stability, abdominal muscle control
- Lumbar (L1-L5): Hip and leg movement
- Sacral (S1-S5): Bowel, bladder, and sexual functions
Injuries to the thoracic, lumbar, or sacral regions can lead to paraplegia, with differing implications:
- Thoracic level injuries (T1-T12): Can cause complete paralysis of the legs, loss of abdominal muscle control, and impaired trunk balance. The higher the thoracic injury, the more extensive the impact.
- Lumbar level injuries (L1-L5): May result in some loss of function in the hips and legs but often spare abdominal muscle control. Depending on the exact level, one may retain some leg movement.
- Sacral level injuries (S1-S5): Primarily affect bowel, bladder, and sexual functions, with variable impact on leg movement and sensation.
The American Spinal Injury Association (ASIA) Impairment Scale helps classify the severity of spinal cord injuries:
- ASIA A: Complete loss of motor and sensory function below the injury level
- ASIA B: Some sensation remains below the injury level, but no motor function
- ASIA C: Motor function remains below the injury level, but more than half of key muscles are weak
- ASIA D: Motor function remains below the injury level, with at least half of key muscles having good strength
- ASIA E: Motor and sensory functions are normal
Understanding the nuances of how injury location and severity impact paraplegia allows for more personalised rehabilitation and clearer expectations for recovery.
Causes of Paraplegia
Paraplegia causes can be broadly classified into traumatic and non-traumatic:
- Traumatic causes: Result from a sudden, severe impact or injury to the spinal cord
- Non-traumatic causes: Develop over time due to an illness or underlying medical condition
Traumatic Causes
Traumatic paraplegia causes involve a forceful blow or cut to the spinal cord, leading to immediate paralysis. Common examples include:
- Motor vehicle accidents: High-impact collisions can fracture, dislocate, or crush vertebrae, causing spinal cord trauma
- Falls: Falling from heights or severe slips and falls can lead to spinal fractures and paralysis
- Sports injuries: High-risk activities like diving, skiing, or horseback riding pose risks of spinal cord trauma
- Violence: Gunshot or stab wounds can directly sever or compress the spinal cord
The abrupt, drastic nature of traumatic injuries makes them a leading cause of paraplegia, especially among younger individuals.
Non-Traumatic Causes
Non-traumatic paraplegia causes stem from medical conditions that gradually compress or damage the spinal cord, such as:
- Spinal tumours: Cancerous growths can press on the spinal cord, causing progressive paraplegia
- Spinal infections: Bacterial or viral infections like meningitis or epidural abscesses can inflame and damage the spinal cord
- Vascular disorders: Spinal strokes or arteriovenous malformations can disrupt blood supply to the spinal cord
- Degenerative disorders: Conditions like multiple sclerosis, amyotrophic lateral sclerosis (ALS), or spinal muscular atrophy can lead to spastic paraplegia
While the onset may be more gradual, non-traumatic paraplegia causes can be equally debilitating and require prompt medical attention to prevent further damage.
What are common risk factors for developing paraplegia?
While not all risk factors are controllable, understanding them can guide preventive measures and lifestyle modifications. These risk factors include:
- Participating in high-risk sports or activities without proper safety precautions
- Having a family history of degenerative neurological conditions
- Unsafe driving behaviors that raise the likelihood of motor vehicle accidents
- Occupations involving physical labor, heights, or heavy machinery
- Weakened immune system or chronic health conditions that make one susceptible to infections
Signs and Symptoms of Paraplegia
Paraplegia symptoms can vary depending on the level and extent of spinal cord damage but commonly include:
- Loss of movement in the legs: Difficulty or inability to voluntarily move the lower extremities, ranging from weakness to complete paralysis.
- Sensory changes: Loss of sensation, numbness, tingling, or burning sensations in the legs and lower body.
- Bladder and bowel dysfunction: Difficulty controlling urination and bowel movements due to impaired neural signals.
- Spasticity: Involuntary muscle spasms or stiffness in the legs, a hallmark of spastic paraplegia.
- Pain: Neuropathic pain or hypersensitivity in the affected areas due to altered sensory pathways.
Other signs may include:
- Impaired sexual function
- Difficulty regulating blood pressure and body temperature
- Skin breakdown or pressure sores due to lack of sensation and mobility
- Muscle atrophy from disuse
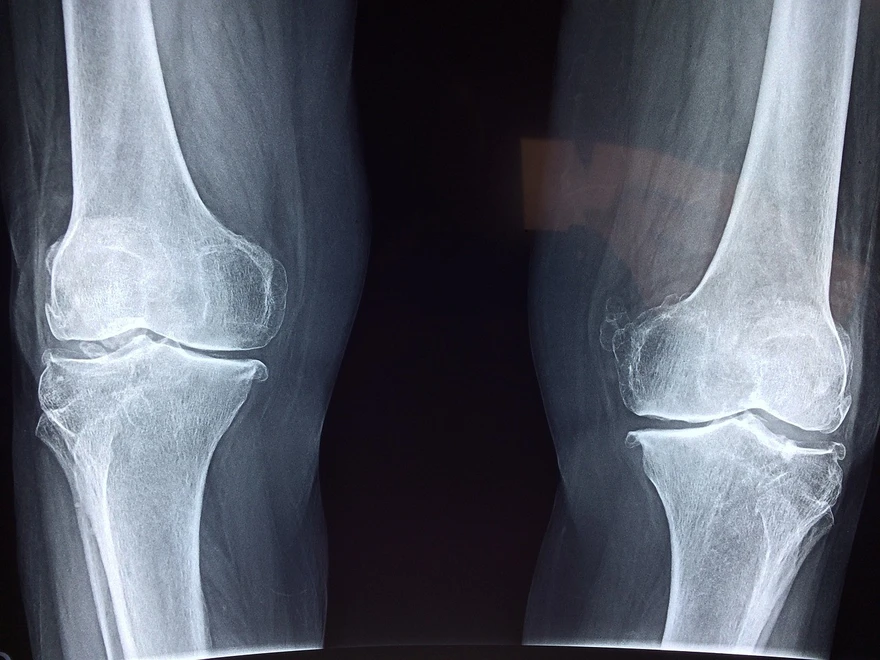
Diagnosis and Tests
Diagnosing paraplegia involves a comprehensive medical evaluation to assess the extent and location of the spinal cord injury. Initial assessments check for movement, sensation and neurological function below the level of injury. Imaging tests are crucial for identifying the cause and severity of paraplegia:
- X-rays help detect vertebral fractures and misalignments
- CT scans provide detailed images of bone fractures, bleeding and spinal stenosis
- MRI scans reveal spinal cord injuries, herniated discs and vascular issues
Additional diagnostic procedures may include:
- Somatosensory evoked potential (SSEP) to evaluate nerve pathway function
- Myelography for enhanced visualisation of the spinal cord
A thorough medical history and physical examination are also key components of the diagnostic process. Your doctor will assess paraplegia symptoms such as loss of movement, altered sensation, and changes in bladder and bowel function. Prompt diagnosis is essential for timely treatment and rehabilitation. If you experience concerning symptoms after a spinal injury, seek immediate medical attention for an accurate evaluation.
Rehabilitation and Treatment Options
Paraplegia rehabilitation focuses on maximising independence through physical therapy, psychological support, adaptive devices and learning new skills for mobility.
Role of Physical Therapy in Recovery
Physical therapy is vital for paraplegia recovery, helping to improve muscle strength and flexibility, enhance mobility and transfers, prevent complications like pressure sores, adapt to assistive devices, and set rehabilitation goals. Regular PT sessions with a skilled therapist can significantly boost function and independence after a spinal cord injury.
Medications and Pain Management
Medications play a key role in managing paraplegia symptoms such as chronic pain, muscle spasms and spasticity, and bladder and bowel dysfunction. Common treatments include analgesics, antispasmodics, and medications for neurogenic bladder and bowel. Work closely with your doctor to find the right combination for optimal symptom control.
Assistive Devices That Help Mobility
Assistive technology enhances mobility and independence with paraplegia. Essential devices include manual or power wheelchairs, walkers and crutches, orthotics like braces, and aids for reaching and gripping. An occupational therapist can help select and adapt equipment to your individual needs, ensuring safe and efficient mobility at home and in the community.
Is Surgery Ever an Option?
Surgery may be recommended for certain spinal cord injuries causing paraplegia, especially for decompression of the spinal cord, stabilisation of fractures, and relieving pressure on nerves. The goal of surgery is to prevent further damage, reduce pain and improve neurological function when possible. Your medical team will determine if you're a candidate.
Living with Paraplegia: Daily Life & Emotional Well-being
Adapting to life with paraplegia involves significant physical and emotional adjustments. It's normal to experience a range of feelings, from grief and anger to anxiety and depression. Prioritising your mental health is just as important as physical rehabilitation.
Some strategies for maintaining emotional well-being include:
- Seeking counseling or therapy
- Joining a support group for people with spinal cord injuries
- Staying connected with loved ones
- Engaging in enjoyable hobbies and social activities
- Practicing stress-management techniques like meditation
Remember, it's okay to ask for help. Surround yourself with a strong support system of family, friends, and healthcare professionals who can provide practical and emotional assistance as you navigate this new chapter. With time and support, it is possible to live a fulfilling life with paraplegia.
Support Systems and Resources
Building a robust support network is essential when living with paraplegia. In addition to family and friends, your healthcare team is a vital resource. This may include physiatrists (rehabilitation doctors), physical and occupational therapists, psychologists or counsellors, social workers, and nurses specialising in spinal cord injury care. Take advantage of community resources like peer support groups, adaptive sports programmes, vocational rehabilitation services, and independent living centres.
Remember, you're not alone on this journey. Reach out for help when needed and don't hesitate to explore the many resources available. Connecting with others who understand the challenges of spinal cord injury can provide encouragement and practical advice as you adapt to life with paraplegia.
Prognosis and Long-term Outlook
The prognosis for paraplegia depends on factors like the level and completeness of injury. Some recovery of function may be possible.
Can You Recover from Paraplegia?
While complete recovery is rare, many people with paraplegia experience some improvement in function over time. Factors influencing recovery include the severity of the spinal cord injury, the level of injury, and the timing and intensity of rehabilitation.
Even without full recovery, it's possible to lead a meaningful and productive life with paraplegia.
Advances in Spinal Cord Injury Treatment
Researchers are making exciting progress in developing new treatments for spinal cord injuries, including:
- Stem cell therapies to promote nerve regeneration
- Neuroprotective drugs to minimize secondary injury
- Advanced rehabilitation techniques using robotics and virtual reality
While still experimental, these advances offer hope for improved outcomes in the future.
Living a Full Life with Paraplegia
A spinal cord injury may change your life, but it doesn't define you. People with paraplegia can pursue fulfilling careers, enjoy relationships and family life, travel and explore the world, and stay active with adaptive sports.
Conclusion
Paraplegia rehabilitation involves a comprehensive approach to maximising function, independence and quality of life after spinal cord injury. By working closely with your healthcare team, utilizing support resources, and maintaining a hopeful outlook, it's possible to thrive with paraplegia. Remember, Metropolis Healthcare's expert diagnostic services are here to support you on your journey to living your best life.
FAQs
What's the difference between paraplegia and tetraplegia?
Paraplegia refers to paralysis affecting the legs and lower body, typically due to a spinal cord injury below the neck. Tetraplegia, also known as quadriplegia, involves paralysis of all four limbs and is caused by cervical spinal cord damage.
What's the difference between paraplegia and hemiplegia?
While paraplegia is paralysis of both legs, hemiplegia is weakness or paralysis on one side of the body. Hemiplegia more commonly results from conditions like stroke or brain injuries rather than spinal cord damage.
What is hereditary spastic paraplegia?
Hereditary spastic paraplegia is a group of rare genetic disorders causing progressive weakness and stiffness in the legs. Unlike paraplegia from a spinal cord injury, HSP develops gradually due to nerve degeneration.
Can Paraplegia Be Temporary?
In some cases, paraplegia can be temporary, such as with incomplete spinal cord injuries or spinal shock. With rehabilitation, some individuals may regain function over time. However, for many people with paraplegia, the paralysis is permanent.



1744887454.webp)